More Than Just a Gut Feeling
Have you ever felt “butterflies” in your stomach before a big event? This common sensation is a perfect example of the remarkable link between our gut and our brain. Scientists are now discovering that this connection, known as the gut-brain axis, plays a significant role in many health conditions, including Parkinson’s Disease (PD). For a long time, PD was considered a brain-centric disorder, but cutting-edge research suggests that its origins and progression may be deeply tied to the trillions of microorganisms living in our digestive system. This community of bacteria, fungi, and viruses is called the gut microbiome.
The Microbiome’s Role: An Unseen Conductor
The gut microbiome isn’t just a passive resident; it’s an active participant in our health. It’s involved in digestion, vitamin production, and training our immune system. Researchers have found that individuals with PD often have a significantly different gut microbiome composition compared to healthy people. Specifically, they tend to have a lower diversity of bacterial species and an imbalance in the ratio of certain bacterial types. This imbalance, called dysbiosis, is a key area of study.
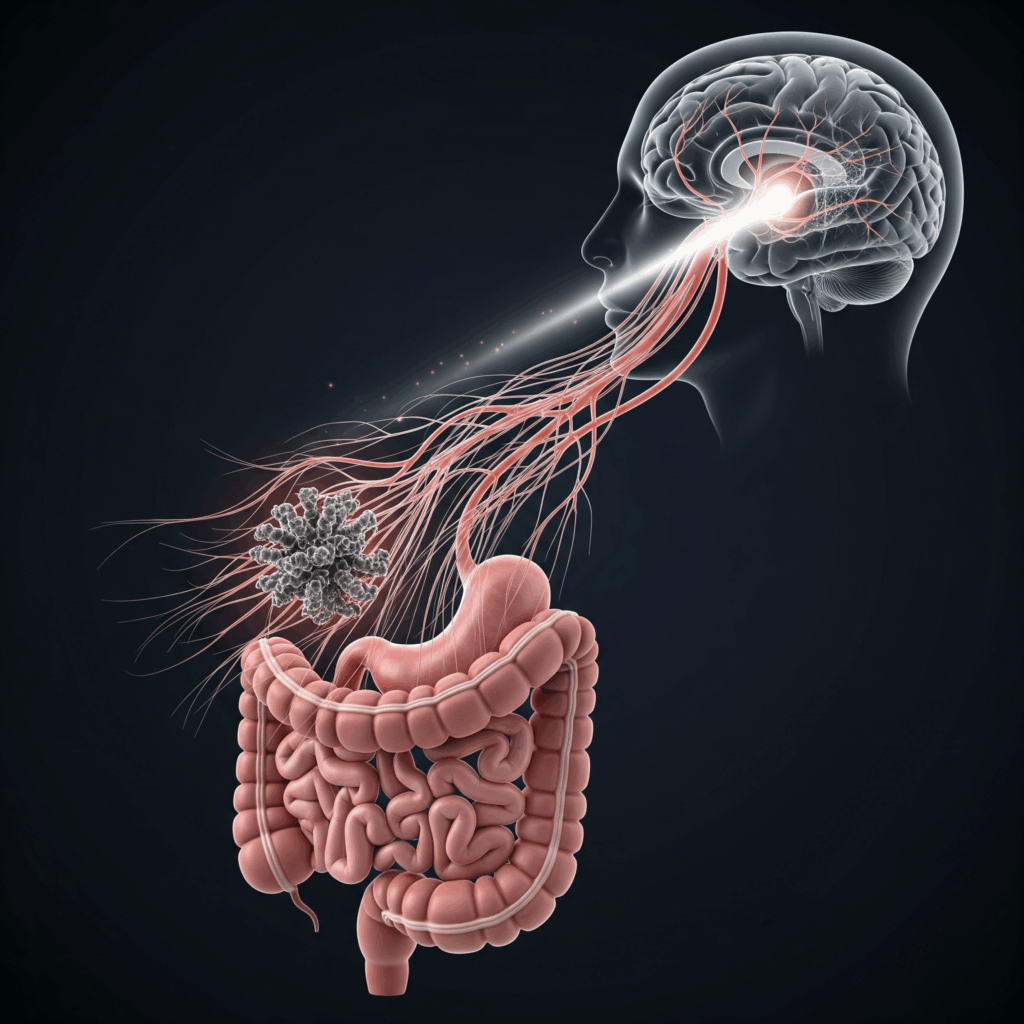
The Parkinson’s Paradox: The Gut as the Starting Point?
One of the most intriguing hypotheses about PD is that the disease might actually begin in the gut, not the brain. The theory, known as the Braak’s hypothesis, suggests that a pathogenic agent or trigger might first enter the body through the gut. This could cause the misfolding of a protein called alpha-synuclein. This misfolded protein then forms clumps, or Lewy bodies, which are a hallmark of PD. According to this theory, these Lewy bodies could then “climb” the vagus nerve—a major communication pathway connecting the gut and the brain—and eventually reach the brain, causing the characteristic motor symptoms of PD.
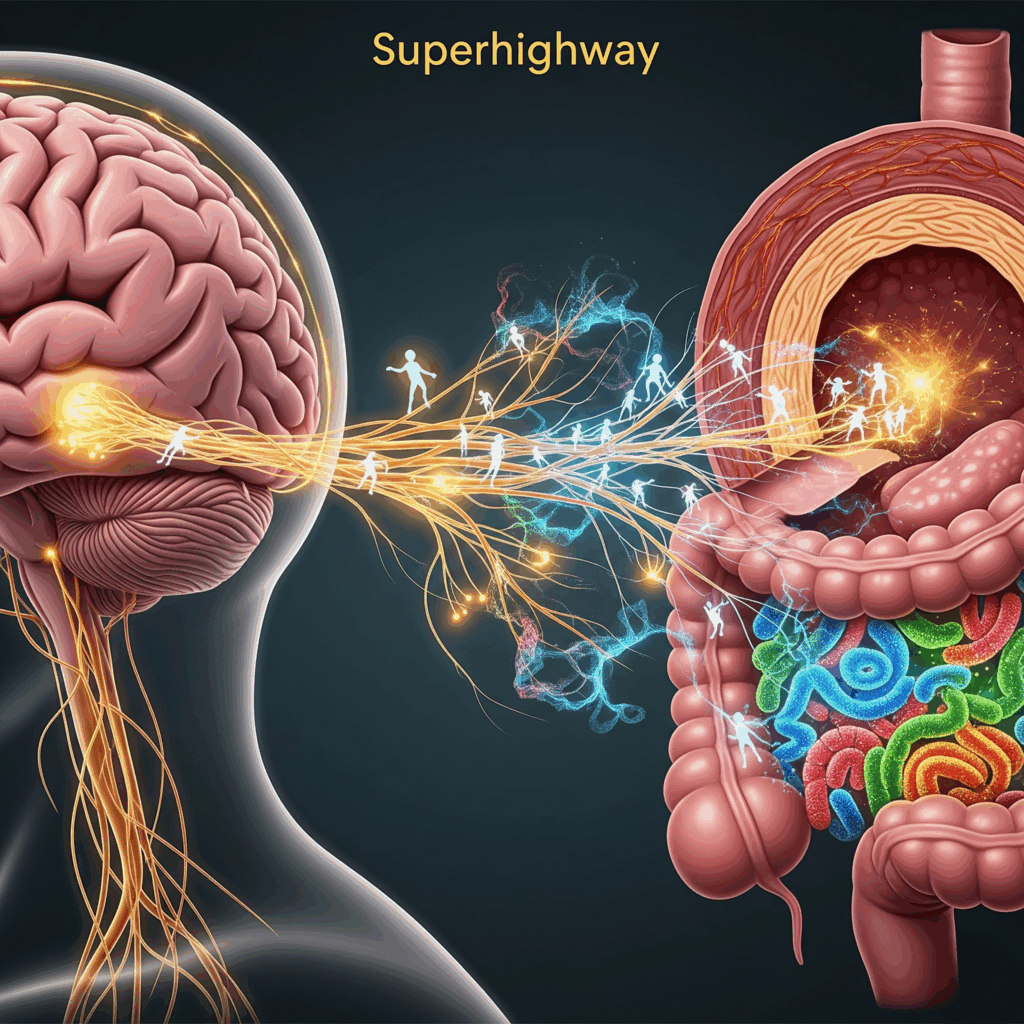
How Does the Microbiome Influence the Gut-Brain Axis?
The gut microbiome communicates with the brain in several ways:
- Vagus Nerve: This direct neural pathway acts as a two-way street, transmitting signals from the gut to the brain and vice versa.
- Immune System: The gut is the largest immune organ in the body. An unhealthy microbiome can lead to inflammation, which can send signals to the brain and contribute to neuroinflammation, a known factor in PD progression.
- Metabolites: Gut bacteria produce a vast array of chemicals, including short-chain fatty acids (SCFAs) like butyrate, which have anti-inflammatory properties and are crucial for gut health. They also produce neurotransmitters like dopamine and serotonin, which can influence mood and motor function.
The Future of Treatment: A Gut-First Approach?
Understanding the gut-brain connection opens up exciting new avenues for PD research and potential treatments. Instead of solely focusing on the brain, scientists are exploring therapies that target the gut microbiome. These could include:
- Probiotics and Prebiotics: Introducing beneficial bacteria (probiotics) or the foods that feed them (prebiotics) to restore a healthy gut balance.
- Fecal Microbiota Transplants (FMT): Transferring a healthy microbiome from a donor to a person with PD, though this is still highly experimental.
- Dietary Interventions: A diet rich in fiber, fruits, and vegetables can promote a diverse and healthy microbiome, potentially slowing PD progression.
The gut-brain connection in PD is a rapidly evolving field, challenging our traditional understanding of this complex disease. It highlights the incredible interdependence of our body’s systems and offers new hope for more effective treatments in the future.
Reference
The Vagus Nerve Hypothesis: Braak, H., et al. (2003). Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiology of Aging, 24(2), 197-211.
Gut Microbiome Dysbiosis in PD: Keshavarzian, A., et al. (2015). Gut dysbiosis in Parkinson’s disease. Movement Disorders, 30(13), 1755-1763.
Alpha-Synuclein and the Gut: Sampson, T. R., et al. (2016). Gut Microbiota Regulate Motor Deficits and Neuroinflammation in a Model of Parkinson’s Disease. Cell, 167(6), 1461-1473.e12.
Short-Chain Fatty Acids and Neuroinflammation: Erny, D., et al. (2015). Host-microbe interactions: Impact on CNS myelination. Science, 349(6250), aab3425.
https://www.parkinson.org/blog/awareness/gut-brain-connection: The Gut-Brain Connection in Parkinson’s Disease https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2024.1348279/full: The Gut-Brain Connection in Parkinson’s Disease
Leave a Reply